As demonstrated in the BEGIN clinical trial program
Tresiba® (insulin degludec) reduced A1C in adults with type 2 diabetes1
Tresiba® met A1C efficacy noninferiority endpoints in 7 out of 7 trials vs insulin glargine U-1001
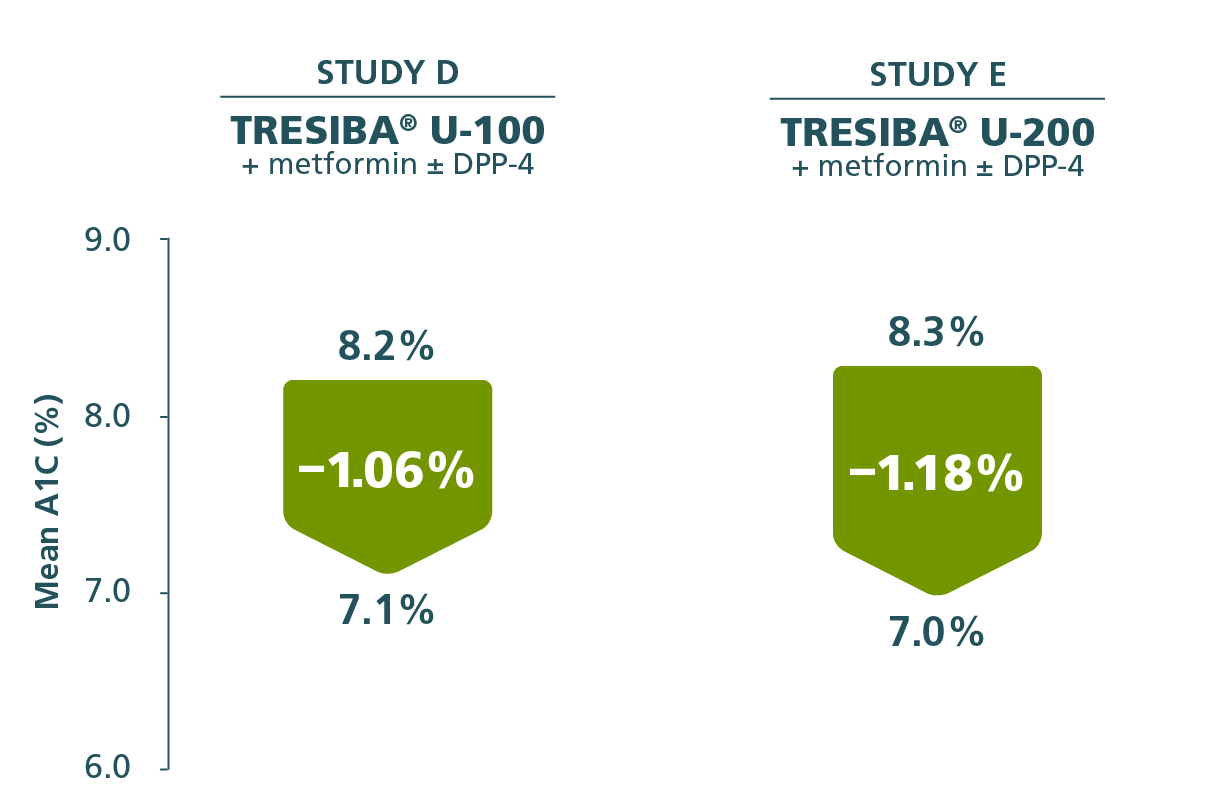
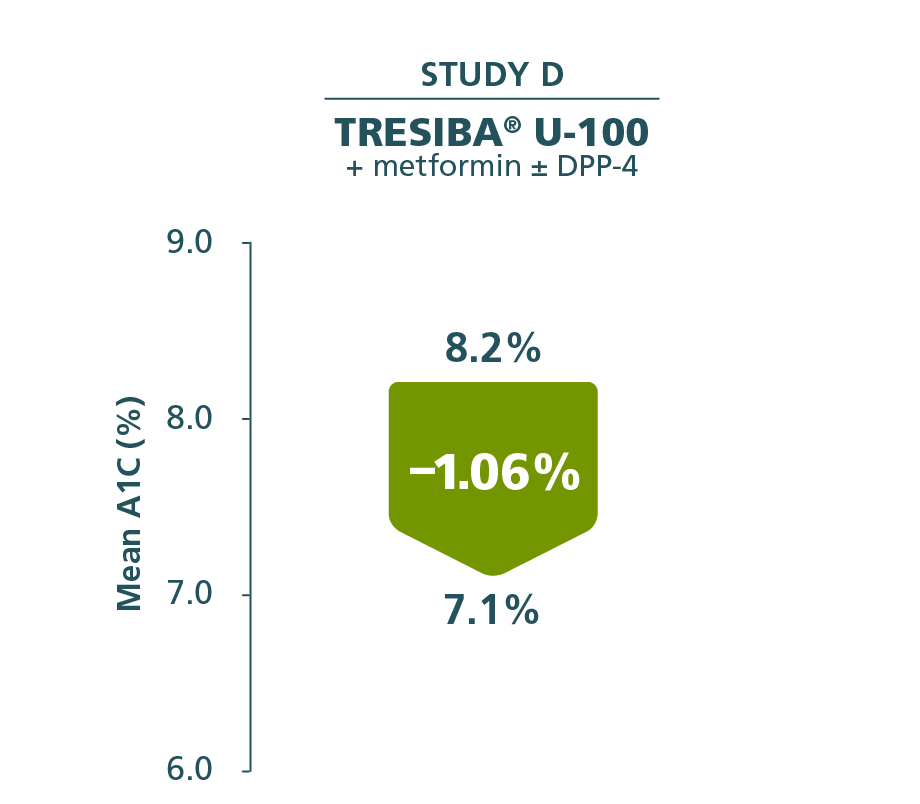
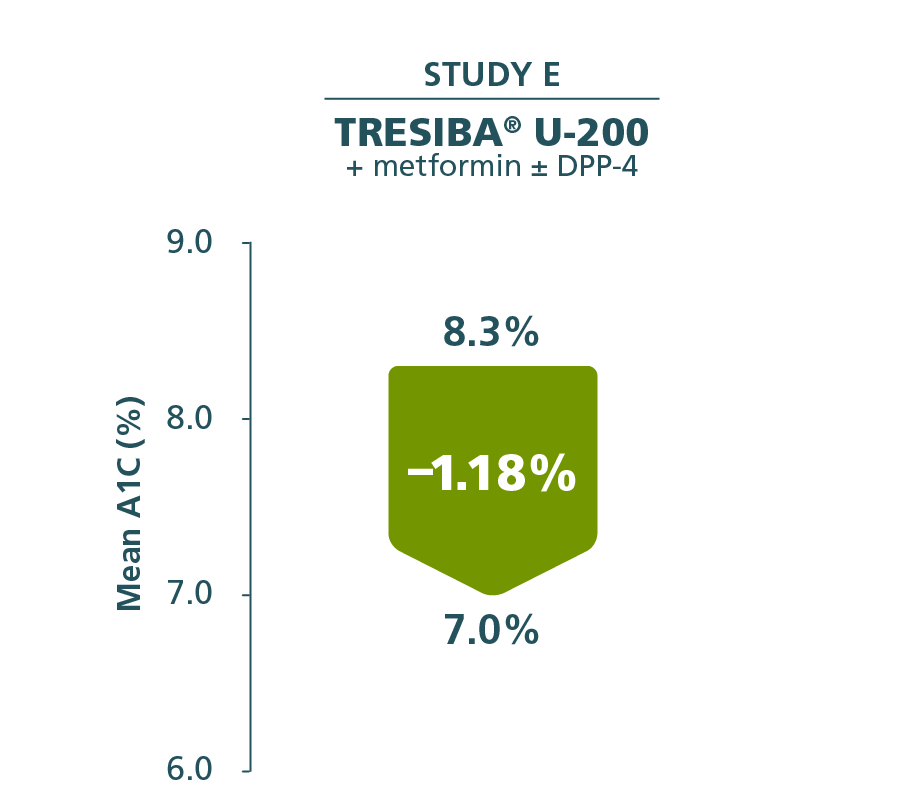
A1C reductions with Tresiba®1
Adults with T2D
Comparator mean change from baseline
Insulin glargine U-100 +
metformin ± DPP-4
Baseline: 8.2%
End of trial: 7.0%
Reduction: –1.15%
Insulin glargine U-100 +
metformin ± DPP-4
Baseline: 8.2%
End of trial: 6.9%
Reduction: –1.22%
Adults with T2D
Comparator mean change from baseline
Insulin glargine U-100 +
metformin ± DPP-4
Baseline: 8.2%
End of trial: 7.0%
Reduction: –1.15%
Adults with T2D
Comparator mean change from baseline
Insulin glargine U-100 +
metformin ± DPP-4
Baseline: 8.2%
End of trial: 6.9%
Reduction: –1.22%
- At Week 52, the difference in A1C reduction from baseline for Tresiba® and insulin glargine U-1001:
- Study D, 0.09% (95% CI, –0.04%; 0.22%)
- At Week 26, the difference in A1C reduction from baseline for Tresiba® U-200 and insulin glargine U-1001:
- Study E, 0.04% (95% CI, –0.11%; 0.19%)
- A1C results were similar between Tresiba® and insulin glargine U-100 in the other 4 clinical trials1
- The prespecified noninferiority margin (0.4%) was met in all 7 clinical trials1
See how Tresiba® was studied in adult and pediatric patients with T1D1

Secondary endpoint
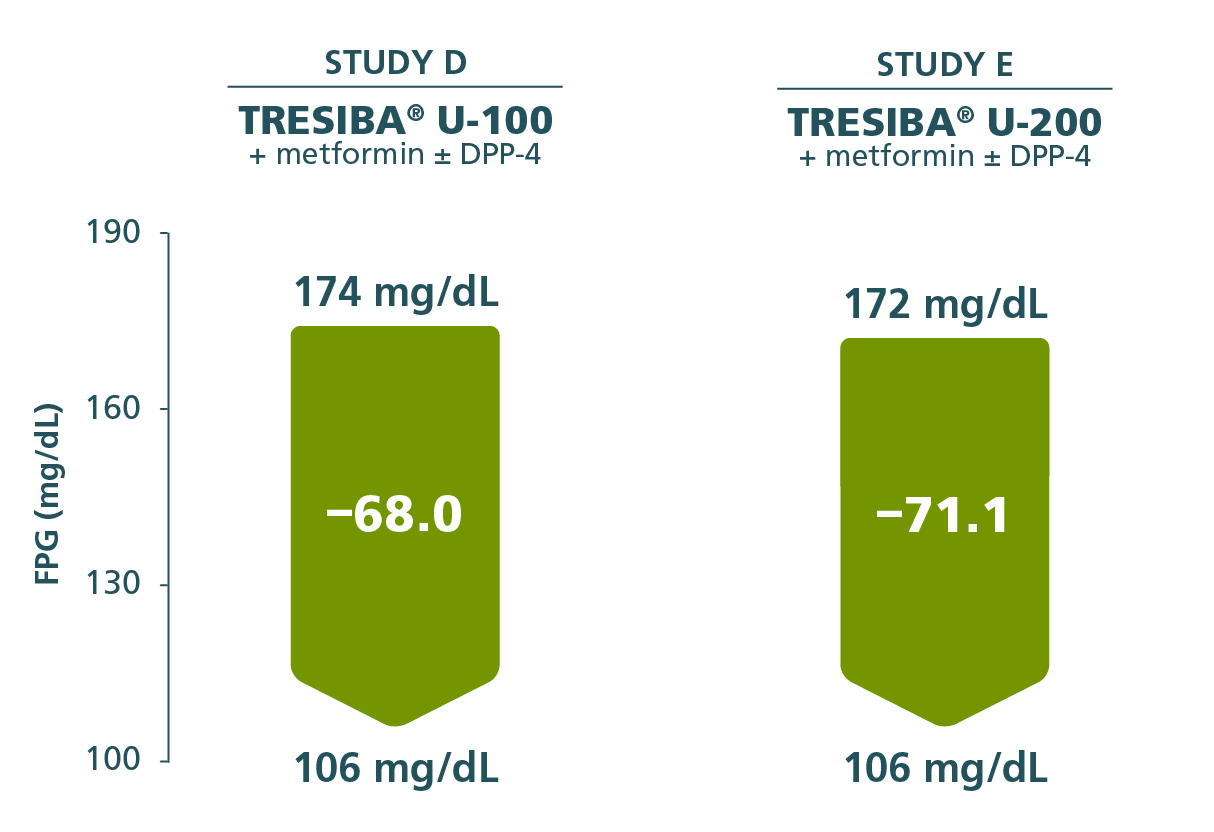
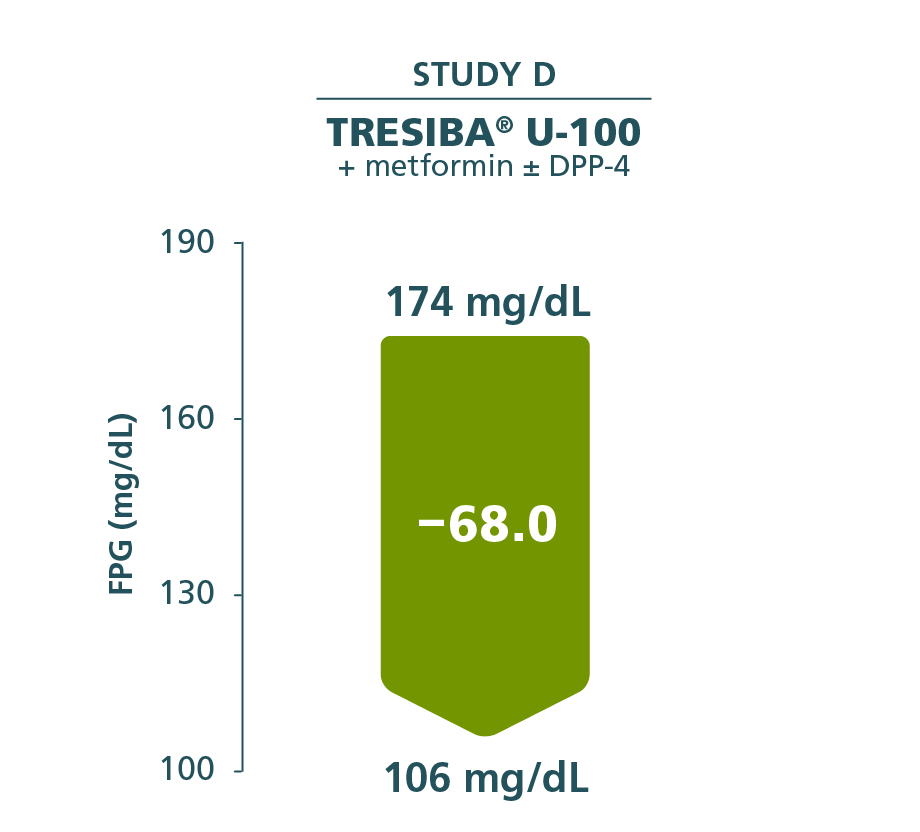
FPG reductions with Tresiba®1
Adults with T2D
Comparator mean change from baseline
Insulin glargine U-100 +
metformin ± DPP-4
Baseline: 174 mg/dL
End of trial: 115 mg/dL
Reduction: –60.2 mg/dL
Insulin glargine U-100 +
metformin ± DPP-4
Baseline: 174 mg/dL
End of trial: 113 mg/dL
Reduction: –63.5 mg/dL
Adults with T2D
Comparator mean change from baseline
Insulin glargine U-100 +
metformin ± DPP-4
Baseline: 174 mg/dL
End of trial: 115 mg/dL
Reduction: –60.2 mg/dL
Adults with T2D
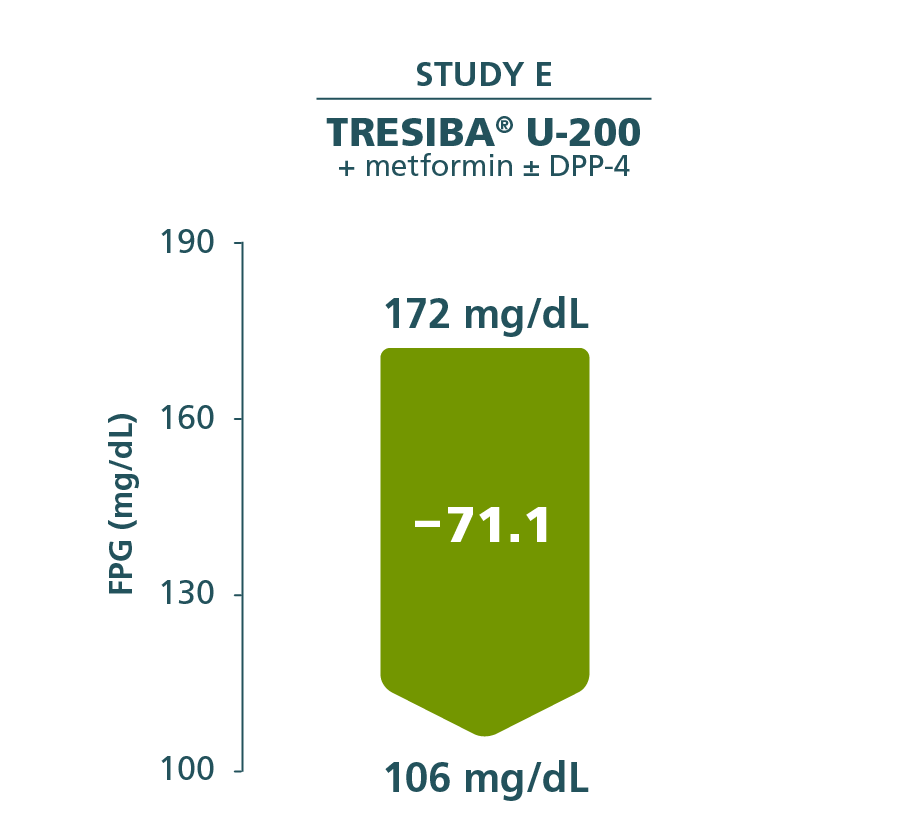
Comparator mean change from baseline
Insulin glargine U-100 +
metformin ± DPP-4
Baseline: 174 mg/dL
End of trial: 113 mg/dL
Reduction: –63.5 mg/dL
- FPG results were similar between Tresiba® and insulin glargine U-100 in the other 4 clinical trials
Additional efficacy endpoint in Studies D and E: FPG reduction from baseline through Week 26 (Study E) or Week 52 (Study D)2,3
In the BEGIN clinical trials
Hypoglycemia incidence rates were comparable among Tresiba® and other basal insulins1
Percentage of patients with type 2 diabetes who experienced at least 1 episode of severe Novo Nordisk–defined hypoglycemiaa,b
0% to 4.5% for severe hypoglycemiaa
28.5% to 80.9% for Novo Nordisk–defined hypoglycemiab (OADs and/or basal bolus)
aSevere hypoglycemia: an event requiring assistance of another person to actively administer carbohydrate, glucagon, or other resuscitative actions.
bNovo Nordisk–defined hypoglycemia: a severe hypoglycemia event or an event where laboratory or self-measured glucose calibrated to plasma was <56 mg/dL or where whole blood glucose was <50 mg/dL (ie, with or without the presence of hypoglycemic symptoms).
Study designs
Study D
Insulin-naïve adults with type 2 diabetes1,2
Patients randomized: Tresiba® (n=773); insulin glargine U-100 (n=257).
Study design: 52-week, randomized, open-label, multicenter trial comparing the efficacy and safety of once-daily Tresiba® U-100 and once-daily insulin glargine U-100, both with metformin with or without a DPP-4 inhibitor. Basal insulin was titrated weekly to an FPG target of 70 to 90 mg/dL according to mean prebreakfast self-measured blood glucose (SMBG) values (mean of 3 consecutive days).
Primary endpoint: Change in A1C from baseline after 52 weeks of treatment.
Other efficacy assessments: Change from baseline in FPG, SMBG, and A1C <7% responders.
Mean end-of-trial basal insulin doses: Tresiba®, 56 units; insulin glargine U-100, 58 units.
Study E
Insulin-naïve adults with type 2 diabetes1,3
Patients randomized: Tresiba® (n=228); insulin glargine U-100 (n=229).
Study design: 26-week, randomized, open-label, multicenter trial comparing the efficacy and safety of once-daily Tresiba® U-200 and once-daily insulin glargine U-100, both with metformin with or without a DPP-4 inhibitor. Basal insulin was titrated weekly to an FPG target of 70 to 90 mg/dL according to mean prebreakfast SMBG values (mean of 3 consecutive days).
Primary endpoint: Change in A1C from baseline after 26 weeks of treatment.
Secondary confirmatory endpoints: Number of treatment-emergent confirmed hypoglycemic episodes, change from baseline in FPG, within-subject variability as measured by coefficient of variation, and frequency of participants achieving A1C <7% without confirmed hypoglycemic episodes.
Mean end-of-trial basal insulin doses: Tresiba®, 59 units; insulin glargine U-100, 62 units.
View the mechanism of protraction video to see how Tresiba® works
Important Safety Information for Tresiba®
Contraindications
- Tresiba® is contraindicated during episodes of hypoglycemia and in patients with hypersensitivity to insulin degludec or any of the excipients in Tresiba®
Warnings and Precautions
- Never Share a Tresiba® FlexTouch® Pen, Needle, or Syringe Between Patients, even if the needle is changed. Patients using Tresiba® vials should never share needles or syringes with another person. Sharing poses a risk for transmission of blood-borne pathogens.
- Hyperglycemia or Hypoglycemia with Changes in Insulin Regimen: Changes in an insulin regimen (e.g., insulin strength, manufacturer, type, or injection site or method of administration) may affect glycemic control and predispose to hypoglycemia or hyperglycemia. Repeated insulin injections into areas of lipodystrophy or localized cutaneous amyloidosis have been reported to result in hyperglycemia; and a sudden change in the injection site (to an unaffected area) has been reported to result in hypoglycemia. Make any changes to a patient’s insulin regimen under close medical supervision with increased frequency of blood glucose monitoring. Advise patients who have repeatedly injected into areas of lipodystrophy or localized cutaneous amyloidosis to change the injection site to unaffected areas and closely monitor for hypoglycemia. Adjustments in concomitant anti-diabetic treatment may be needed.
- Hypoglycemia: Hypoglycemia is the most common adverse reaction of insulin, including Tresiba®. Severe hypoglycemia can cause seizures, may be life-threatening or cause death. Hypoglycemia can impair concentration ability and reaction time; this may place the patient and others at risk in situations where these abilities are important (e.g., driving or operating other machinery). Hypoglycemia can happen suddenly and symptoms may differ in each patient and change over time in the same patient. Symptomatic awareness of hypoglycemia may be less pronounced in patients with longstanding diabetes, in patients with diabetic neuropathy, using drugs that block the sympathetic nervous system (e.g., beta-blockers) or who experience recurrent hypoglycemia. The long-acting effect of Tresiba® may delay recovery from hypoglycemia compared to shorter-acting insulins.
Risk Factors for Hypoglycemia: The risk of hypoglycemia generally increases with intensity of glycemic control. The risk of hypoglycemia after an injection is related to the duration of action of the insulin and, in general, is highest when the glucose lowering effect of the insulin is maximal. As with all insulins, the glucose lowering effect time course of Tresiba® may vary among different patients or at different times in the same patients and depends on many conditions, including the area of injection as well as the injection site blood supply and temperature. Other factors which may increase the risk of hypoglycemia include changes in meal pattern, changes in level of physical activity, or changes to concomitant drugs. Patients with renal or hepatic impairment may be at higher risk of hypoglycemia. Patients and caregivers must be educated to recognize and manage hypoglycemia. In patients at higher risk for hypoglycemia and patients who have reduced symptomatic awareness of hypoglycemia, increased frequency of blood glucose monitoring is recommended. - Hypoglycemia Due to Medication Errors: Accidental mix-ups between insulin products have been reported. To avoid medication errors between Tresiba® and other insulins, always instruct patients to always check the insulin label before each injection. To avoid dosing errors and potential overdose, never use a syringe to remove Tresiba® from the Tresiba® FlexTouch® disposable insulin prefilled pen.
- Hypersensitivity Reactions: Severe, life-threatening, generalized allergy, including anaphylaxis, can occur with insulins, including Tresiba®. If hypersensitivity reactions occur, discontinue Tresiba®; treat per standard of care and monitor until symptoms and signs resolve.
- Hypokalemia: All insulins, including Tresiba®, cause a shift in potassium from the extracellular to intracellular space, possibly leading to hypokalemia. Untreated hypokalemia may cause respiratory paralysis, ventricular arrhythmia, and death. Monitor potassium levels in patients at risk for hypokalemia and treat if indicated.
- Fluid Retention and Heart Failure with Concomitant Use of PPAR-gamma Agonists: Fluid retention and heart failure can occur with concomitant use of thiazolidinediones (TZDs), which are PPAR-gamma agonists, and insulin, including Tresiba®. Patients should be observed for signs and symptoms of heart failure. If heart failure occurs, dosage reduction or discontinuation of the TZD must be considered.
Adverse Reactions
- Adverse reactions commonly associated with Tresiba® are hypoglycemia, allergic reactions, injection site reactions, lipodystrophy, pruritus, rash, edema, and weight gain.
Drug Interactions
- There are certain drugs that may cause clinically significant drug interactions with Tresiba®.
- Drugs that may increase the risk of hypoglycemia: antidiabetic agents, ACE inhibitors, angiotensin II receptor blocking agents, disopyramide, fibrates, fluoxetine, monoamine oxidase inhibitors, pentoxifylline, pramlintide, salicylates, somatostatin analog (e.g., octreotide), sulfonamide antibiotics, GLP-1 receptor agonists, DPP-4 inhibitors, and SGLT-2 inhibitors
- Drugs that may decrease the blood glucose lowering effect: atypical antipsychotics (e.g., olanzapine and clozapine), corticosteroids, danazol, diuretics, estrogens, glucagon, isoniazid, niacin, oral contraceptives, phenothiazines, progestogens (e.g., in oral contraceptives), protease inhibitors, somatropin, sympathomimetic agents (e.g., albuterol, epinephrine, terbutaline), and thyroid hormones
- Drugs that may increase or decrease the blood glucose lowering effect: alcohol, beta-blockers, clonidine, lithium salts, and pentamidine
- Drugs that may blunt the signs and symptoms of hypoglycemia: beta-blockers, clonidine, guanethidine, and reserpine
Please click here for Tresiba® Prescribing Information.
Important Safety Information for Tresiba®
Contraindications
- Tresiba® is contraindicated during episodes of hypoglycemia and in patients with hypersensitivity to insulin degludec or any of the excipients in Tresiba®
Warnings and Precautions
- Never Share a Tresiba® FlexTouch® Pen, Needle, or Syringe Between Patients, even if the needle is changed. Patients using Tresiba® vials should never share needles or syringes with another person. Sharing poses a risk for transmission of blood-borne pathogens.
- Hyperglycemia or Hypoglycemia with Changes in Insulin Regimen: Changes in an insulin regimen (e.g., insulin strength, manufacturer, type, or injection site or method of administration) may affect glycemic control and predispose to hypoglycemia or hyperglycemia. Repeated insulin injections into areas of lipodystrophy or localized cutaneous amyloidosis have been reported to result in hyperglycemia; and a sudden change in the injection site (to an unaffected area) has been reported to result in hypoglycemia. Make any changes to a patient’s insulin regimen under close medical supervision with increased frequency of blood glucose monitoring. Advise patients who have repeatedly injected into areas of lipodystrophy or localized cutaneous amyloidosis to change the injection site to unaffected areas and closely monitor for hypoglycemia. Adjustments in concomitant anti-diabetic treatment may be needed.
- Hypoglycemia: Hypoglycemia is the most common adverse reaction of insulin, including Tresiba®. Severe hypoglycemia can cause seizures, may be life-threatening or cause death. Hypoglycemia can impair concentration ability and reaction time; this may place the patient and others at risk in situations where these abilities are important (e.g., driving or operating other machinery). Hypoglycemia can happen suddenly and symptoms may differ in each patient and change over time in the same patient. Symptomatic awareness of hypoglycemia may be less pronounced in patients with longstanding diabetes, in patients with diabetic neuropathy, using drugs that block the sympathetic nervous system (e.g., beta-blockers) or who experience recurrent hypoglycemia. The long-acting effect of Tresiba® may delay recovery from hypoglycemia compared to shorter-acting insulins.
Risk Factors for Hypoglycemia: The risk of hypoglycemia generally increases with intensity of glycemic control. The risk of hypoglycemia after an injection is related to the duration of action of the insulin and, in general, is highest when the glucose lowering effect of the insulin is maximal. As with all insulins, the glucose lowering effect time course of Tresiba® may vary among different patients or at different times in the same patients and depends on many conditions, including the area of injection as well as the injection site blood supply and temperature. Other factors which may increase the risk of hypoglycemia include changes in meal pattern, changes in level of physical activity, or changes to concomitant drugs. Patients with renal or hepatic impairment may be at higher risk of hypoglycemia. Patients and caregivers must be educated to recognize and manage hypoglycemia. In patients at higher risk for hypoglycemia and patients who have reduced symptomatic awareness of hypoglycemia, increased frequency of blood glucose monitoring is recommended. - Hypoglycemia Due to Medication Errors: Accidental mix-ups between insulin products have been reported. To avoid medication errors between Tresiba® and other insulins, always instruct patients to always check the insulin label before each injection. To avoid dosing errors and potential overdose, never use a syringe to remove Tresiba® from the Tresiba® FlexTouch® disposable insulin prefilled pen.
- Hypersensitivity Reactions: Severe, life-threatening, generalized allergy, including anaphylaxis, can occur with insulins, including Tresiba®. If hypersensitivity reactions occur, discontinue Tresiba®; treat per standard of care and monitor until symptoms and signs resolve.
- Hypokalemia: All insulins, including Tresiba®, cause a shift in potassium from the extracellular to intracellular space, possibly leading to hypokalemia. Untreated hypokalemia may cause respiratory paralysis, ventricular arrhythmia, and death. Monitor potassium levels in patients at risk for hypokalemia and treat if indicated.
- Fluid Retention and Heart Failure with Concomitant Use of PPAR-gamma Agonists: Fluid retention and heart failure can occur with concomitant use of thiazolidinediones (TZDs), which are PPAR-gamma agonists, and insulin, including Tresiba®. Patients should be observed for signs and symptoms of heart failure. If heart failure occurs, dosage reduction or discontinuation of the TZD must be considered.
Adverse Reactions
- Adverse reactions commonly associated with Tresiba® are hypoglycemia, allergic reactions, injection site reactions, lipodystrophy, pruritus, rash, edema, and weight gain.
Drug Interactions
- There are certain drugs that may cause clinically significant drug interactions with Tresiba®.
- Drugs that may increase the risk of hypoglycemia: antidiabetic agents, ACE inhibitors, angiotensin II receptor blocking agents, disopyramide, fibrates, fluoxetine, monoamine oxidase inhibitors, pentoxifylline, pramlintide, salicylates, somatostatin analog (e.g., octreotide), sulfonamide antibiotics, GLP-1 receptor agonists, DPP-4 inhibitors, and SGLT-2 inhibitors
- Drugs that may decrease the blood glucose lowering effect: atypical antipsychotics (e.g., olanzapine and clozapine), corticosteroids, danazol, diuretics, estrogens, glucagon, isoniazid, niacin, oral contraceptives, phenothiazines, progestogens (e.g., in oral contraceptives), protease inhibitors, somatropin, sympathomimetic agents (e.g., albuterol, epinephrine, terbutaline), and thyroid hormones
- Drugs that may increase or decrease the blood glucose lowering effect: alcohol, beta-blockers, clonidine, lithium salts, and pentamidine
- Drugs that may blunt the signs and symptoms of hypoglycemia: beta-blockers, clonidine, guanethidine, and reserpine
Please click here for Tresiba® Prescribing Information.
References:
- Tresiba [package insert]. Plainsboro, NJ: Novo Nordisk Inc; July 2022.
- Zinman B, Philis-Tsimikas A, Cariou B, et al. Diabetes Care. 2012;35(12):2464-2471.
- Gough SCL, Bhargava A, Jain R, Mersebach H, Rasmussen S, Bergenstal RM. Diabetes Care. 2013;36(9):2536-2542.