Diagnosing acquired hemophilia
When unexplained bleeding with no previous history occurs, urgent laboratory testing to aid in diagnosis is recommended. Approximately 70% of acquired hemophilia (AH) patients experience severe, unexplained bleeding at diagnosis, with widely varying bleeding patterns.1
Diagnosing acquired hemophilia
When unexplained bleeding with no previous history occurs, urgent laboratory testing to aid in diagnosis is recommended. Approximately 70% of acquired hemophilia (AH) patients experience severe, unexplained bleeding at diagnosis, with widely varying bleeding patterns.1
How do patients with AH present?
Acquired hemophilia signs and symptoms
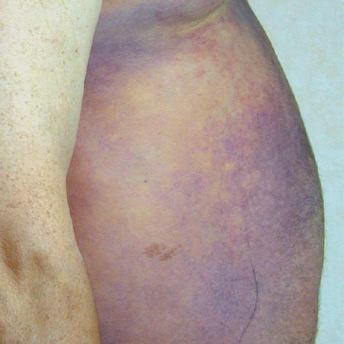
Purpura (bruising) and soft-tissue hemorrhage2
Bleeding sites atypical of congenital hemophilia3
Gastrointestinal, urological, or retroperitoneal bleeding4,5
Prolonged bleeding following surgery2
Compartment syndrome (compression of blood vessels and nerves)3
Isolated prolonged activated partial thromboplastin time (aPTT)2
Purpura (bruising) and soft-tissue hemorrhage2
Bleeding sites atypical of congenital hemophilia3
Gastrointestinal, urological, or retroperitoneal bleeding4,5
Prolonged bleeding following surgery2
Compartment syndrome (compression of blood vessels and nerves)3
Isolated prolonged activated partial thromboplastin time (aPTT)2

Importance of early diagnosis
Patients frequently experience delays in diagnosis for acquired hemophilia. Prompt diagnosis is vital to minimize a patient’s risk of bleeding complications and avoid non-essential invasive procedures.2
Parameter
Parameter
Normal
range7,a
Normal range6,a
Acquired
hemophilia6
Acquired
hemophilia3
aPTT
25-38
seconds
25-38 seconds
Above
normal
Above normal
PT
11-13
seconds
11-13 seconds
Normal
Normal
FVIII
50%-150%
activity
50%-150% activity
Below
normal
Below normal
aPTT=activated partial thromboplastin time; PT=prothrombin time.
aNormal ranges may vary among different laboratories.
Consult a hematologist immediately if lab results show an unexplained, isolated, prolonged aPTT.3,4,7
Consult a hematologist immediately if lab results show an unexplained, isolated, prolonged aPTT.4,6
Confirm an acquired hemophilia diagnosis through lab testing
Explore an interactive clinical pathway for patients with acquired hemophilia
Review an example of treating acquired hemophilia in the emergency department.
References:
- Knoebl P, Marco P, Baudo F, et al; EACH2 Registry Contributors. Demographic and clinical data in acquired hemophilia A: results from the European Acquired Haemophilia Registry (EACH2). J Thromb Haemost. 2012;10(4):622-631.
- Collins PW, Percy CL. Advances in the understanding of acquired haemophilia A: implications for clinical practice. Br J Haematol. 2010;148(2):183-194.
- Giangrande P. Acquired Hemophilia: Revised Edition: Treatment of Hemophilia No. 38. Montréal, Québec: World Federation of Hemophilia; 2012:1-2.
- Tiede A, Collins P, Knoebl P, et al. International recommendations on the diagnosis and treatment of acquired hemophilia A. Haematologica. 2020;105(7):1-16.
- Collins PW, Hirsch S, Baglin TP, et al; for UK Haemophilia Centre Doctors’ Organisation. Acquired hemophilia A in the United Kingdom: a 2-year national surveillance study by the United Kingdom Haemophilia Centre Doctors’ Organisation. Blood. 2007;109(5):1870-1877.
- Introduction to normal values (reference ranges). In: Wallach J, ed. Interpretation of Diagnostic Tests. 8th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2007:3-25.